Engorgement and Why it Happens
It’s normal and expected that your breasts undergo many changes throughout your lactation journey. I always ask my clients if their breasts grew or their areola became darker in pregnancy, which is a good sign that the hormones are doing their job to prepare for lactation! It’s also very normal for the breasts to become very heavy, swollen, and full when mature milk first starts to come in (generally on days 3-5 post-birth), and lactating breasts may feel full and lumpy at times and soft at others. Sounds fun, doesn’t it?!
What is Engorgement?
This is probably a term you have heard before, but what does engorgement really mean? Engorgement is defined as breast pain, firmness, and swelling that is usually uncomfortable. While it can happen at any time throughout a lactation journey, it most commonly occurs with the onset of mature milk production or if the breasts go too long without emptying.
What Causes Engorgement?
Recent research has just been released from the Academy of Breastfeeding Medicine (ABM), reshaping how lactation specialists view and treat engorgement. The ABM reports that engorgement is most often related to tissue swelling and inflammation caused by fluid accumulation in the breast tissue, not in the milk ducts. This means that engorgement is not usually related to higher milk volumes!
This is especially true in the first two weeks after delivery- the breasts swell to an uncomfortable level as oxytocin and prolactin are hard at work shifting colostrum to mature milk in higher volumes. Generally, with this kind of engorgement, the body will self-regulate, and symptoms will resolve in a few days with minimal intervention.
If engorgement is experienced after the supply has been regulated, then it is generally due to a surplus of milk production or gaps between feedings that are too long, causing milk to pool to an uncomfortable level. Generally, if my clients are experiencing consistent engorgement past the first few weeks postpartum, I would assess and treat them for oversupply issues.
How Do I Get Rid of Engorgement?
If you are in the first 2 weeks after giving birth, the focus for engorgement management is minimizing tissue inflammation, not aggressively trying to remove milk or emptying the breasts, as this will only worsen the situation!
Here are my top tips:
Feed your baby on demand (when they show hunger cues) and allow them to do what they do best, remove milk and soften the breasts. Babies are the most effective form of milk removal, and the goal is to allow them to regulate your supply by telling your body how much milk they need. By feeding them whenever they are hungry, your body will naturally regulate how much milk it’s making to meet their needs.
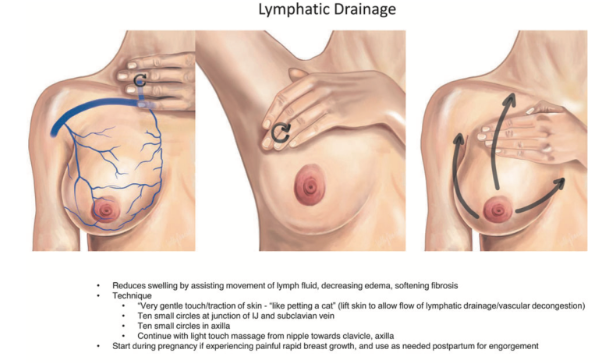
While a lot of extra pumping may temporarily relieve the pressure in the breasts, you are telling your body to make more milk than your baby needs. You are also increasing inflammation in the tissues, so the cycle continues. This is why doing a lot of extra pumping is not recommended for engorgement treatment.Focus on gentle lymphatic drainage techniques rather than firm massaging of the breast tissue:
Taking NSAID pain relievers such as ibuprofen can help minimize discomfort and reduce inflammation. If the engorgement is severe, you can also consider applying cool packs to the breasts after feeding sessions to decrease swelling as well. Just be sure not to apply ice to your nipples, as this can disrupt the nerve signals that are imperative in the lactation cycle.
If you are ever uncomfortably full and your baby is not ready to eat, hand expression is a great way to relieve pressure without providing extra stimulation. Some women find that warm showers or baths can also passively help flow the milk. Sometimes the breasts are so full (literally rock hard) the baby can have difficulty grasping and latching to the breast- this is the perfect time to hand express for a few minutes to soften the tissue to the point where the baby can latch.
If you are experiencing engorgement past the first few weeks postpartum, you should be evaluated by a lactation specialist to determine if oversupply needs to be managed with an individualized and carefully monitored plan of care.
Please note that if you develop any flu-like symptoms or a fever along with engorgement symptoms, you should reach out to your healthcare provider, as these are concerning signs of mastitis that may require medical attention.
After having a baby, your body goes through so many changes that can be uncomfortable or even shocking. I encourage you to trust your body and know that it has many powerful tools to balance itself and provide what you and your baby need. If you are worried about any changes or cycles your body may be experiencing, please reach out to our team of professionals, as we are here to provide guidance and reassurance as needed!
Resources
- Mitchell, K. (2022). Academy of Breastfeeding Medicine Clinical Protocol #36: The mastitis ... Academy of Breastfeeding Medicine. Retrieved October 2, 2022, from https://www.bfmed.org/assets/ABM%20Protocol%20%2336.pdf